National Heart Centre Singapore will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
When Hearts Need Extra Care: Congenital Heart Disease And Pregnancy

Contributed By Asst Prof Yan Limin, Consultant, Cardiology
Congenital heart disease (CHD) is present in approximately 1% of live births, and can range from simple lesions such as atrial septal defects (ASD) or ventricular septal defects (VSD) to more complex conditions that can involve multiple lesions. With advancements in medical care and surgical techniques, most children born with CHD will survive to childbearing age, even those with complex lesions. NHCS manages the largest cohort of approximately 4,000 adult congenital heart disease (ACHD) patients in Singapore.
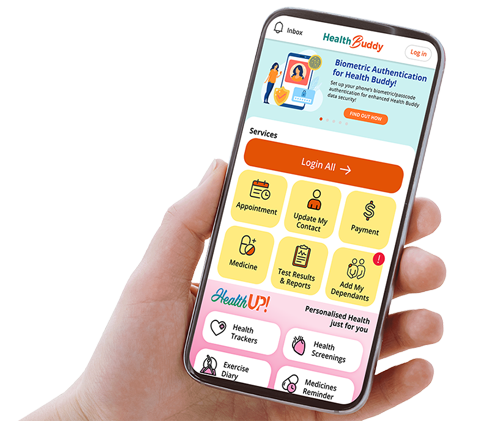
Pregnancy induces significant physiological changes in the cardiovascular system, to support the increased metabolic demands of both mother and foetus. These changes begin as early as the first trimester and include an increase in blood volume and heart rate (see Fig. 1).

For women with pre-existing heart disease, these changes can pose challenges as their cardiovascular system may not adapt effectively. Patients may be at increased risk of heart failure, arrhythmias (abnormal heart rhythms), miscarriages or pre-term labour. Therefore, it is important to optimise cardiac function and manage any co-existing medical conditions before conception.
The European Society of Cardiology (ESC) has recently released their latest guidelines – the 2025 ESC Guidelines for the management of cardiovascular disease and pregnancy. In these guidelines, they have updated the modified World Health Organization (WHO) Classification of maternal cardiovascular risk during pregnancy. This classification helps guide our management of cardiac conditions during pregnancy. Different types of CHDs can fall anywhere on the spectrum from low risk to high risk depending on the nature of the underlying condition (see table below).

NHCS-SGH Cardiac Joint Clinic (CJC)
The multidisciplinary clinic offers comprehensive care for pregnant patients with pre-existing heart conditions. While ACHD is among the most commonly managed conditions, the clinic also supports patients with acquired or inherited cardiac disorders. During each visit, patients are jointly reviewed by both a cardiologist and an obstetrician, allowing for real-time discussion and personalised care planning tailored to the patient's specific cardiac and obstetric needs.
For ACHD patients specifically, they may require more frequent antenatal (pregnancy) visits and non-invasive cardiac imaging, with regular review and assessment of cardiac medications. These visits also facilitate planning for appropriate foetal cardiac screening and discussions about the potential implications for offspring in cases of inherited or genetic cardiac conditions.
A case of simple CHD (Ventricular Septal Defect) and pregnancy
Ventricular septal defect (VSD) is a defect between the two lower chambers of the heart (left and right ventricle). The increased blood volume during pregnancy can result in an increase in blood flow across the VSD and subsequently dilatation of the left-sided chambers. However, overall risk for an uncomplicated VSD without pulmonary hypertension (high blood pressure in the lungs) is low. Patients often do not require additional monitoring or intervention during delivery. Vaginal delivery is recommended unless otherwise indicated from an obstetric point of view.

Ms X is 30 years old with a history of a small VSD. She does not present any cardiac symptoms. Her last cardiac imaging prior to pregnancy was a transthoracic echocardiogram (TTE), an ultrasound scan of the heart, which showed a small VSD with non-haemodynamically significant left to right shunt, normal left ventricular (LV) size and function. This was her first pregnancy. She was referred to the CJC and seen once during each trimester with a follow-up TTE during her third trimester to monitor her cardiac function. She had an uncomplicated spontaneous normal vaginal delivery at term and was discharged on day three.
A case of complex CHD (Pentalogy of Fallot) and pregnancy
Pentalogy of Fallot is a rare form of cyanotic CHD involving Tetralogy of Fallot and in this patient's case - an atrial septal defect (ASD). During pregnancy, there may be increased stress on the right ventricle and more deoxygenated blood may flow across the ASD and VSD into the systemic circulation (the body's main blood supply system that delivers oxygen to all organs), making the patient more cyanotic.

Ms S is 32 years old with unrepaired Pentalogy of Fallot (Tetralogy of Fallot with an ASD). During her pregnancy, she was seen monthly at the CJC throughout her pregnancy, to allow close monitoring of her cardiac function and oxygen levels, and for the obstetricians to closely monitor foetal growth. She was planned for elective caesarean for obstetric reasons due to her previous caesarean (for twin pregnancy). The scheduled caesarean was supported by both cardiothoracic and obstetric anaesthetists, with cardiologist and cardiothoracic surgeons on standby. The caesarean procedure went smoothly without complications and baby was born at 37 weeks.
Pregnancy in CHD is a journey that starts preconception. With appropriate counselling and careful planning, most women with CHD can safely navigate pregnancy and childbirth.
REFERENCES
1. Birth defects in Singapore: 1994-2000. K H Tan et al. Singapore Medical Journal. 2005;46(10): 545
© 2025 SingHealth Group. All Rights Reserved.