What is - Pulmonary Arterial Hypertension
Pulmonary arterial hypertension (PAH) is a condition of high lung pressure in the blood vessels leading from the heart to the lung. There are many different types of pulmonary hypertension, but PAH is the most important type.
Sometimes, the exact cause of PAH is not known. In some rare cases, PAH can be inherited.
PAH is more often diagnosed in people with certain diseases. These include:
- portal hypertension (due to liver problems)
- connective tissue disease such as systemic sclerosis
- congenital heart disease
- human immunodeficiency virus (HIV)
Symptoms of Pulmonary Arterial Hypertension
The physical impact or the signs and symptoms of pulmonary arterial hypertension are caused by decrease in oxygen-rich supply throughout the body and the effects of overworked and tired heart.
Some of the most common symptoms include:
- shortness of breath during physical or normal activities
- feeling tired at all times or chronic fatigue
- dizziness especially when climbing stairs or prolonged standing up
- chest discomfort
- palpitations
- syncope
- swollen ankles or legs
- dry cough
PAH can affect anyone of any age, sex or race. It is however, more common in women aged between 30 and 50 years old. As symptoms of PAH resembles those of other conditions, it is often not easy to diagnose.
Pulmonary Arterial Hypertension - Causes and Risk Factors
Pulmonary arterial hypertension belongs to Pulmonary Hypertension Group 1 based on the classification schema published in the 2013 5th World Symposium in Pulmonary Hypertension held in NICE. It has several subgroups (see Table 1) such as idiopathic, heritable or familial, related to drugs and toxins or associated with certain conditions such as connective tissue disease, HIV infection, portal hypertension, congenital heart disease or schistosomiasis.
| Table 1: Updated Classification of Pulmonary Hypertension |
1. Pulmonary arterial hypertension 1.1 Idiopathic PAH 1.2 Heritable PAH 1.2.1 BMPR2 1.2.2 ALK-1, ENG, SMAD9, CAV1, KCNK3 1.2.3 Unknown 1.3 Drug and toxin induced 1.4 Associated with: 1.4.1 Connective tissue disease 1.4.2 HIV infection 1.4.3 Portal hypertension 1.4.4 Congenital heart diseases 1.4.5 Schistosomiasis 1′ Pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis 1′′ Persistent pulmonary hypertension of the newborn (PPHN) |
Source: Abridged version from Simonneau et al. Classification of Pulmonary Hypertension
In PAH, the pulmonary arteries constrict and become increasingly narrow. Progression of the disease is characterised by inflammation and remodeling of the blood vessels. The endothelial cells multiply, the smooth muscle cells increase in size and number and the fibroblasts cells multiply. Consequently, the walls of these vessels become thicker and less flexible. This narrowing of the pulmonary arteries restricts blood flow to the lungs and causes an increase in resistance, which causes the blood pressure in the arteries to rise.

Over time, the right heart is enlarged. This explains why the impact of PAH is not limited to the arteries in the lungs but has a direct impact on the heart. In some cases, over a period of time, the right heart will start to enlarge and decompensate. As a result, less blood will circulate through the lungs, picking up less oxygen overall. This may make people with PAH feel tired and breathless. If PAH is not treated, the right heart will start to fail.
Connective Tissue Disease-Associated Pulmonary Arterial Hypertension (CTD-PAH)
Connective tissue disease-associated pulmonary arterial hypertension (CTD-PAH) describes a group of autoimmune diseases that can cause PAH.
Examples include systemic sclerosis (scleroderma) and systemic lupus erythematosus (SLE) or mixed connective tissue disease.
By far, systemic sclerosis is the main cause of CTD-associated PAH. It is important to screen for CTD-PAH because there may be no symptoms or very mild symptoms at the early stage.
Diagnosis of Pulmonary Arterial Hypertension
Diagnosis typically starts with a physical examination by a doctor, assessing your medical history and routine tests. Other tests recommended may include:
- Chest X-ray
- Electrocardiogram (ECG)
- Computed Tomography (CT) lungs
- Echocardiogram
- Lung function tests
- Right heart catherisation
Treatment for Pulmonary Arterial Hypertension
The treatment options for patients with PAH can be broadly classified into three main groups – general measures, supportive measures and PAH-specific therapies.
-
General Measures
General measures include the avoidance of strenuous activities, the avoidance of pregnancy through careful family planning and the use of appropriate contraception, and timely vaccination for influenza and pneumococcus. -
Supportive Measures
Supportive measures include the use of oxygen for patients who require long-term oxygen therapy, the use of diuretics to help relieve organ congestion and the use of oral anticoagulation to help to prevent thromboembolism to the lungs. -
PAH-specific therapy
PAH-specific therapy mainly targets three main pathways. The first pathway targets the Nitric Oxide Pathway including the synthesis of nitric oxide, as well as nitric oxide, soluble guanylate cyclase and cyclic GMP signaling pathway. The drugs in this category include medication such as sildenafil, tadalafil and roiciguat. The second group of medication targets Endothelin Receptors (eg. Bosentan) and the final pathway targets the Prostacyclin Pathway which includes drugs such as inhaled iloprost, iv prostacyclin etc.
Pulmonary Arterial Hypertension - Other Information
Aftercare
Patients living with PAH may not be able to keep up with the active lifestyle they are used to. A task that would normally take an hour may take several days or more. Patients are advised to prioritise their activities and set a realistic goal.
Over-the-counter drugs should be taken with extra care. Some drugs may have interaction with blood thinners such as warfarin whereas sedative drugs can worse hypoxia in patients with PAH. Patients are advised to consult their doctor for advice first.
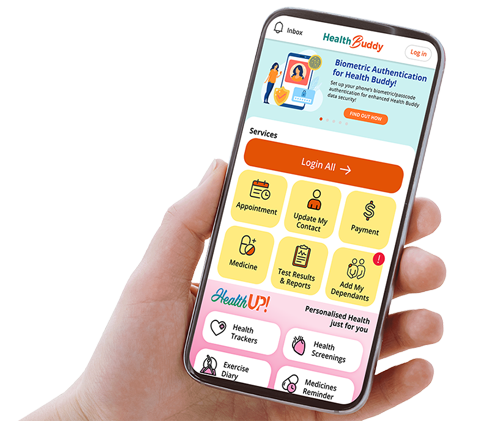
NHCS PAH patients are followed up regularly at the Pulmonary Hypertension Clinic. During the clinic visit, the patient’s response to treatment as well as signs of clinical deterioration will be assessed. Blood tests such as NT-proBNP, liver and kidney function tests are monitored regularly to assess the effects of treatment. An annual echocardiogram and 6-minute walk test are done to assess the effect of treatment on right heart function and patient’s functional capacity.
Pulmonary Arterial Hypertension (video with English subtitles)
Pulmonary Arterial Hypertension (video with Chinese subtitles)
NHCS Pulmonary Hypertension Clinic
NHCS runs a monthly pulmonary hypertension clinic - a joint clinic run by cardiologists from NHCS together with respiratory physicians and rheumatologists from the Singapore General Hospital (SGH) with the assistance of trained and specialised pulmonary hypertension nurses. The pulmonary hypertension clinic provides a comprehensive and seamless care for PAH patients as they enjoy the convenience of seeing three specialists in one clinic session. It also allows the multidisciplinary team to discuss and manage complex PAH patients in the same setting.
The Pulmonary Hypertension Team
| National Heart Centre Singapore Clin Assoc Prof Lim Soo Teik Senior Consultant, Department of Cardiology Clin Asst Prof Tan Ju Le Senior Consultant, Department of Cardiology Asst Prof Victor Chao Senior Consultant, Department of Cardiothoracic Surgery Dr Ruan Wen Consultant, Department of Cardiology Clin Assoc Prof Jonathan Yap Consultant, Department of Cardiology Aidila Binte Ismail Nurse Clinician Sumathy D/O Perumal Senior Staff Nurse Lim Chee Lan Senior Staff Nurse | Singapore General Hospital Dr Andrea Low Head and Senior Consultant, Department of Rheumatology & Immunology Clin Assoc Prof Phua Ghee Chee Head and Senior Consultant, Department of Respiratory & Critical Care Medicine Clin Asst Prof Sewa Duu Wen Senior Consultant, Department of Respiratory & Critical Care Medicine Dr Cassandra Hong Consultant, Department of Rheumatology & Immunology Dr Sue-Ann Ng Consultant, Department of Rheumatology & Immunology |
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.