PRESS RELEASE
The Lancet: Experts call for urgent action to reduce global burden of cardiovascular disease in women by 2030
Peer-reviewed / Meta-analysis / People
- Cardiovascular disease (CVD) is the leading cause of death among women, responsible for 35% of deaths in women per year worldwide, with cardiovascular disease mortality increasing in young women.
- Despite this, CVD among women remains understudied, under-recognised, underdiagnosed, and undertreated, with women under-represented in clinical trials.
- Strategies to tackle inequities in diagnosis, treatment, and prevention of CVD are urgently required.
- The Lancet women and cardiovascular disease Commission outlines 10 ambitious recommendations to improve health outcomes for millions of women around the world and achieve the global targets set.
In the first-ever global report on cardiovascular disease (CVD) in women, researchers call for urgent action to improve care and prevention, fill knowledge gaps, and increase awareness to tackle the worldwide leading cause of death among women. The all-female led Commission report was published in The Lancet and presented during a plenary session at the American College of Cardiology’s 70th Annual Scientific Session (ACC.21).
The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030 is authored by 17 leading experts from 11 countries. The Commission aims to help reduce the global burden of cardiovascular conditions – including heart disease and stroke – that account for 35% of deaths in women worldwide by 2030. The Commission’s calls to urgently address and reduce CVD in women align with the United Nations Sustainable Development Goals (SDGs) which aim to reduce premature deaths from non-communicable diseases, including CVD, by one-third by 2030. [1]
The authors have outlined 10 ambitious recommendations to tackle inequities in diagnosis, treatment, and prevention to reduce CVD in women, including educating health care providers and patients on early detection to prevent heart disease in women; scaling up heart health programs in highly populated and underdeveloped regions; and prioritizing sex-specific research on heart disease in women and intervention strategies.
Professor Roxana Mehran, from Mount Sinai Medical Center, USA, says: “Cardiovascular disease in women remains understudied, under-recognised, under-diagnosed, and under-treated globally. Achieving the important target set by the United Nations requires bold, distinct strategies to not only target factors contributing to CVD but also to identify sex-specific biological mechanisms in women. Making permanent improvements to the worldwide care of women with CVD requires coordinated efforts and partnerships involving policymakers, clinicians, researchers, and the wider community.” [2]
The global burden of cardiovascular disease in women
The Commissioners report data from the 2019 Global Burden of Disease Study [3] for the first time to describe the extent of cardiovascular disease in women worldwide, including disease prevalence, mortality, and risk factors.
In 2019, there were approximately 275 million women around the world with CVD, with global age-standardised prevalence estimated at 6,402 cases per 100,000. The leading cause of death from CVD worldwide in 2019 was ischemic heart disease (47% of CVD deaths), followed by stroke (36% of CVD deaths). There are considerable geographical differences in CVD, with the highest age-standardised prevalence in Egypt, Iran, Iraq, Libya, Morocco, and United Arab Emirates, while the countries with lowest prevalence are Bolivia, Peru, Colombia, Ecuador, and Venezuela.
Although globally the prevalence of CVD in women has been declining, with an overall decrease of 4.3% since 1990, some of the world’s most populous nations have seen an increase in CVD, including China (10% increase), Indonesia (7%), and India (3%). These increases indicate a need for initiatives to expand prevention, diagnosis, and treatment of CVD in women who live in highly populated and industrialising regions.
The highest CVD mortality rates are in Central Asia, Eastern Europe, North Africa, and the Middle East, Oceania and Central Sub-Saharan Africa, where age-standardised mortality exceeds 300 deaths per 100,000 women. High-income Asia Pacific, Australasia, Western Europe, Andean Latin America and High-income North America recorded the lowest rates, with fewer than 130 deaths per 100,000 women. Evidence of important regional trends highlight a need for improved data collection at local and regional levels to effectively prevent, recognise, and treat CVD in women.
CVD risk factors in women
High blood pressure is the greatest risk factor contributing to years of lost life from CVD in women, followed by high body mass index and high LDL cholesterol. While these well-established risk factors might affect women differently than men, there are sex-specific risk factors such as premature menopause and pregnancy related-disorders that must be more widely recognized and prioritized as part of treatment and prevention efforts worldwide.
The Commissioners highlight a number of under-recognised CVD risk factors that also require attention. These include social factors – such as unemployment – linked to anxiety and depression, and disparities based on socioeconomic and cultural status, race, and poverty. Among their recommendations are a greater focus on mental health in clinical practice, and targeted policy work to support low socioeconomic status populations in developed and emerging countries.
Professor Bairey Merz, of the Cedars-Sinai Medical Center, USA, says: “While some risk factors for CVD are similar for women and men, women are more likely to suffer from health disparities due to cultural, political or socioeconomic factors. For instance, some social or religious norms – such as restrictions on participation in sport and physical activities – can contribute to CVD in women, highlighting an urgent need for culturally appropriate initiatives that are tailored to different regions and populations.”
The Commission also highlights the need to increase awareness of CVD risk in women among physicians, scientists, and health care providers, and that there is an unmet need for CVD prediction models that include sex-specific risk factors.
Tailored interventions are urgently needed
Interventions to reduce CVD should be tailored for the most vulnerable populations globally, including women from minority or indigenous populations and those whose roles in society are strongly defined by traditional or religious norms. However, it is also important to reach groups not typically viewed as being at high risk, such as young women – a group in which heart attacks and smoking rates are increasing. In the past decade, 53 (27%) of 195 countries and territories recorded significant decreases in the prevalence of smoking among men, while only 32 (16%) recorded significant reductions for women.
Despite a vital need for knowledge about sex-related differences in optimal treatment and improved outcomes in patients of both sexes, women have long been under-represented in CVD clinical trials. The Commissioners recommend a number of strategies to include more women, including addressing barriers to participation – such as family care issues – adopting more inclusive enrolment criteria, and educating recruitment staff on the importance of involving women in trials.
Professor Liesl Zuhlke, of Red Cross Children’s and Groote Schuur Hospitals and the University of Cape Town, South Africa, says: “The momentum to strive for equity and equality more broadly for women socially and culturally translates to an extraordinary time to channel that same energy into improving women’s health. Being the leading killer of women globally, CVD must take precedence for our attention and action. This Commission’s work is both a starting point and a call to action to mobilise and energise health care professionals, policymakers – and women themselves – to work toward a healthier future.” [2]
The Commissioners acknowledge some limitations to their report. As this was a report aiming to capture sex-related differences in cardiovascular disease, and not a systematic review, a bias towards highlighting evidence for sex-related disparities over neutral findings cannot be excluded. There was only limited assessment of the important distinction between sex and gender in the report, in part because the terms are often used interchangeably in the literature. The limited availability of quality data on transgender women also meant the Commission was unable to investigate cardiovascular health for this group. Overall evidence presented in the report may be dominated by data from white women and developed countries, reflecting the current availability of more robust data from these populations and regions. More research to explore all these factors is needed.
Writing in a Linked Comment, Dr Ana Olga Mocumbi of the Mozambique National Institute of Health, who was not involved in the Commission report, adds, “In the midst of the COVID-19 pandemic, values of human dignity, solidarity, altruism, and social justice should guide our communities to ensure equitable share of wealth and leveraging of efforts towards the reduction of cardiovascular disease burden in women worldwide. The Commission’s recommendations on additional funding for women’s cardiovascular health programmes, prioritisation of integrated care programmes, including combined cardiac and obstetric care, and strengthening of the health systems accords with efforts to bridge the gap for the world’s worst off. Such a shift in women’s cardiovascular care would be a major step towards equity, social justice, and sustainable development.”
NOTES TO EDITORS
The Commission was supported financially by grants from Abbott Vascular, Abiomed, Amgen, AstraZeneca, Bristol Myers Squibb, CSL Behring, Janssen, Medtronic, Orbus Neich, Philips, and Sanofi, who had no role in study design, data collection, data analysis, data interpretation, or writing of this Commission article. The funds were used towards the planning, development, and public launch of the Commission article. None of the authors were paid for their work on the Commission.
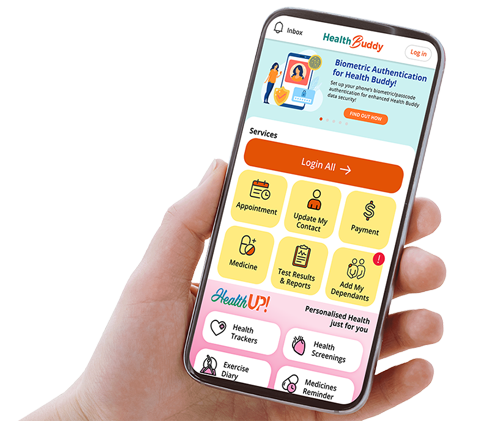
It was conducted by researchers from the Icahn School of Medicine at Mount Sinai, Cedars-Sinai Medical Center, Mayo Clinic, and University of Washington Medical Center, USA, VU University Medical Center Amsterdam, and Radboud University Medical Center, Netherlands, Pontifical Catholic University of Chile, IRCCS San Raffaele Scientific Institute, Italy, University of Sydney, Northern Sydney Local Health District, Kolling Institute, and Macquarie University, Australia, Newcastle University, and Newcastle upon Tyne Hospitals NHS Foundations Trust, UK, National Heart Centre Singapore, Duke-National University of Singapore, Jagiellonian University Medical College, Poland, University of Antioquia, Colombia, Vancouver General Hospital, Canada, and University of Cape Town and Groote Schuur Hospital, South Africa.
The labels have been added to this press release as part of a project run by the Academy of Medical Sciences seeking to improve the communication of evidence. For more information, please see:
http://www.sciencemediacentre.org/wp-content/uploads/2018/01/AMS-press-release-labelling-system-GUIDANCE.pdf if you have any questions or feedback, please contact The Lancet press office
pressoffice@lancet.com
[1] United Nations Sustainable Development Goals (SDGs) 3: Ensure healthy lives and promote well-being for all at all ages:
https://sdgs.un.org/goals/goal3
[2] Quote direct from author and cannot be found in the text of the Article.
[3] Global Burden of Disease Study data is coordinated by the Institute for Health Metrics and Evaluation – an independent global health research centre at the University of Washington, USA.
More information: www.thelancet.com/commissions/women-cardiovascular-disease

English
PressRelease-TL-Women-CVD.pdf